Applying mobility prediction models to real-world patients with major amputations
Selected in Journal of Vascular Surgery by Guillaume Nicaud
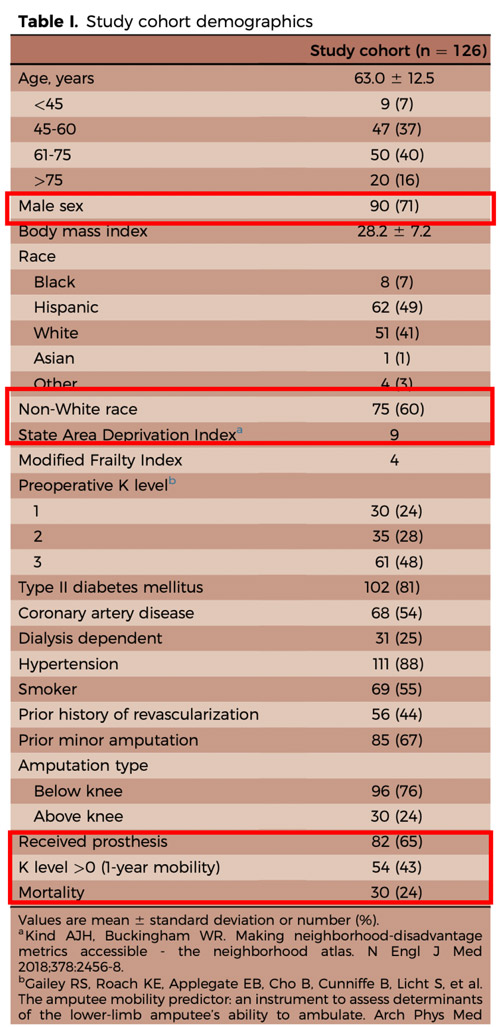
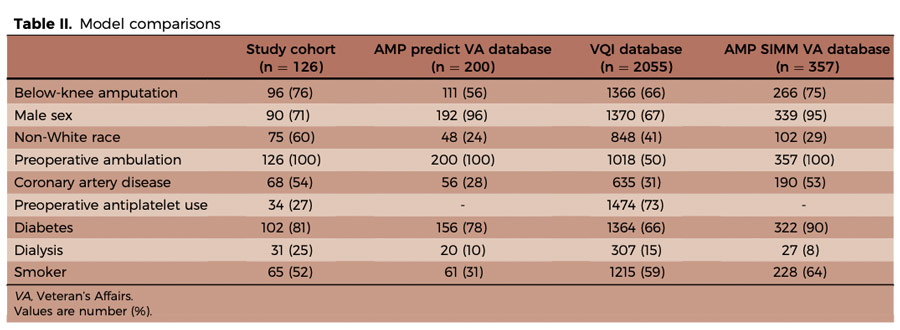
This retrospective multicentre study aimed to evaluate the accuracy of three established predictive models—AmpPredict, AMPSIMM, and VQI—in forecasting one-year mobility after major lower-limb amputation due to ischemia. Conducted across three centres in Fresno, California, the study focused on a socioeconomically disadvantaged population often underrepresented in model development cohorts. Results revealed substantial discrepancies between predicted and actual mobility outcomes, particularly for AMPSIMM and VQI. These findings raise concerns about the applicability of current models in real-world settings and highlight the need for tools better adapted to diverse and vulnerable patient groups.
References:
Authors: Leigh Ann O'Banion, Caroline Runco, Carolina Aparicio, Jessica P. Simons, Karen Woo
Reference: Published online March 21, 2025 - Presented at the Thirty-ninth Annual Meeting of the Western Vascular Society, Colorado Springs, CO, September 7-10, 2024.
DOI: DOI: 10.1016/j.jvs.2025.03.181
Read the abstractBackground:
Major amputations (above the ankle) have increased significantly and are predominantly of vascular origin. However, only 15–30 % of patients regain functional independence. Predictive models exist to estimate post-amputation mobility, but their relevance in real-world, disadvantaged populations remains uncertain.
Objective:
To assess actual mobility at one year using the iBASIC score in patients who underwent major amputation for ischemia and to compare these outcomes with predictions from three established models:
- AmpPredict
- AMPSIMM
- VQI
Methods:
- Retrospective study (2016–2022) in 3 tertiary centers in Fresno, California.
- Included: patients with vascular-related major amputation.
- Excluded: dependent patients, prior contralateral amputation, cognitive impairment.
- Models applied retrospectively using available patient data (worst-case values used when data missing).
Outcomes:
|
Model |
Predicted |
Actual |
Positive Predictive Value |
Negative Predictive Value |
|---|---|---|---|---|
|
AmpPredict |
36.6% |
43% |
58% |
52% |
|
AMPSIMM |
86% |
32% |
33% |
79% |
|
VQI |
76% |
35% |
80% |
50% |
There were notable discrepancies between predicted and actual outcomes, especially in disadvantaged or non-veteran populations.
Get the latest clinical cases and breaking news delivered straight to your inbox!


Discussion:
Predictive models were developed in different populations (e.g., veterans), often with better post-op care and socioeconomic profiles.
The study population had more comorbidities, non-Caucasians, and women — all factors potentially affecting outcomes.
Results suggest these models are not reliable for disadvantaged real-world populations.
Conclusion:
Current predictive models significantly overestimate mobility outcomes after major amputation in real-life, vulnerable populations.
There’s a need to develop or recalibrate models tailored to more diverse and socioeconomically challenged patient groups.