The impact of postoperative dual antiplatelet therapy on outcomes of endovascular therapies in patients with chronic limb-threatening ischemia in the Vascular Quality Initiative–Medicare-linked database
Selected in Journal of Vascular Surgery by Basile Jaulin
Chronic limb-threatening ischemia (CLTI) requires effective post-intervention management to improve limb salvage and survival. However, the best antiplatelet therapy strategy after infrainguinal endovascular treatment remains debated.
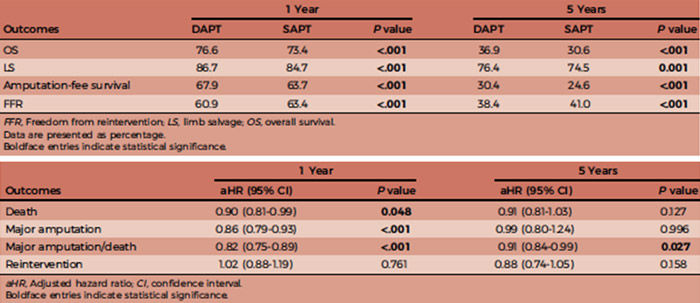
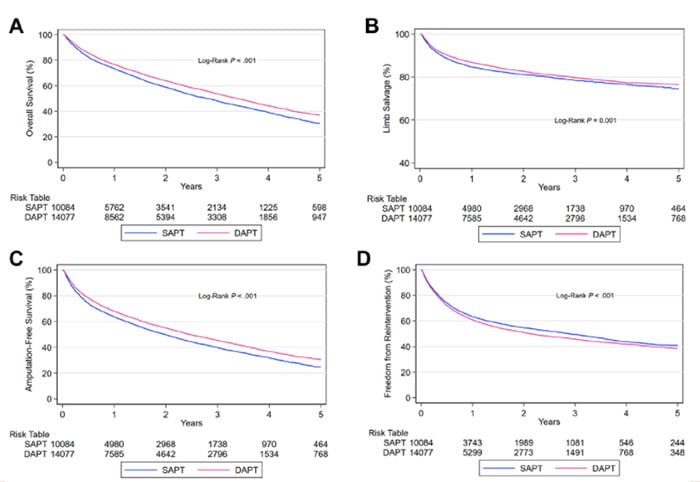
This retrospective study analyses data from the Vascular Quality Initiative–Medicare-linked database (2011–2019) to compare the outcomes of dual antiplatelet therapy (DAPT) versus single antiplatelet therapy (SAPT), focusing on amputation-free survival at 1 and 5 years.
References:
Authors: Sina Zarrintan, Mohammed Hamouda, Munir P. Moacdieh, Mahmoud B. Malas, Ann C. Gaffey
Reference: Published online March 18, 2025
DOI: DOI: 10.1016/j.jvs.2025.03.177
Read the abstractBackground:
Critical limb ischemia (CLI) carries significant risks for limb loss and mortality. The BEST-CLI trial established that revascularisation is recommended, highlighting the roles of both conventional surgery and endovascular approaches.
The choice of antiplatelet therapy (APT) post-revascularisation influences patient outcomes. Dual antiplatelet therapy (DAPT) is currently recommended after certain procedures like myocardial infarction and carotid interventions, but its role in CLI after endovascular treatment is not well defined, with varying levels of supporting evidence.
Objective:
This study aims to compare amputation-free survival (AFS) in patients with chronic limb-threatening ischemia (CLTI) following endovascular intervention, based on whether patients received dual antiplatelet therapy (DAPT) or single antiplatelet therapy (SAPT) postoperatively.
Methods:
Data were collected from the Vascular Quality Initiative (VQI) registry linked to Medicare claims between 2011 and 2019.
Over 1,000 North American centers contribute to the VQI, which includes more than 1.2 million recorded procedures.
Patients with occlusive peripheral arterial disease undergoing infrainguinal endovascular intervention for CLTI were included. Two groups were stratified based on antiplatelet therapy at discharge: SAPT (aspirin or P2Y12 inhibitor) representing 41.7 %, and DAPT (aspirin plus P2Y12 inhibitor) representing 58.3 %.
The primary endpoint was amputation-free survival at 1 year and 5 years. Secondary outcomes included overall survival, freedom from major amputation, and freedom from reintervention.
Statistical analyses included Kaplan-Meier survival curves, log-rank tests, and Cox proportional hazards regression with adjustment for confounders.
Outcomes:
Get the latest clinical cases and breaking news delivered straight to your inbox!


Discussion:
This multicenter retrospective analysis highlights the potential benefit of postoperative dual antiplatelet therapy (DAPT) in patients undergoing endovascular treatment for chronic limb-threatening ischemia (CLTI). The study suggests that DAPT may be associated with improved amputation-free survival compared to single antiplatelet therapy (SAPT).
However, interpretation of these findings requires caution due to the observational and retrospective nature of the data, which may introduce biases such as confounding by indication, treatment selection bias, and limitations inherent to registry and administrative data. Notably, patients selected for DAPT tended to present with more complex clinical profiles, including higher rates of ischemic heart disease and multiple treated vessels, which may have influenced outcomes. The potential impact of P2Y12 inhibitors alone also warrants further investigation, as differences in outcomes between DAPT and P2Y12 monotherapy were not clearly distinguished.
Limitations include incomplete data on the duration and indications for antiplatelet therapy, as well as possible inaccuracies in coding and missing laterality information. Prospective, randomised studies are necessary to confirm these associations and to better define optimal antiplatelet strategies in this high-risk population.
Conclusion:
This large, real-world analysis from the Vascular Quality Initiative linked with Medicare data suggests that postoperative dual antiplatelet therapy may improve amputation-free survival in patients with chronic limb-threatening ischemia undergoing endovascular interventions, compared to single antiplatelet therapy.
However, given the retrospective and observational design, these findings should be interpreted with caution. The potential role of P2Y12 inhibitors alone remains to be clarified.
Prospective randomised trials are essential to confirm these results and to guide optimal antiplatelet management in this vulnerable patient population.