Infrapopliteal peripheral vascular interventions for claudication are performed frequently in the USA and are associated with poor long-term outcomes
Selected in ESVS Journal by Adnan Nseif
As infrapopliteal peripheral vascular interventions (PVIs) for claudication continue to be performed in the USA, this study assessed whether infrapopliteal PVI is linked to worse long-term outcomes than isolated femoropopliteal PVI.
References:
Authors: Sanuja Bosea, Chen Dunb, Alex J. Solomond, James H. Black, Michael S. Contee, Corey A. Kalbaughf, Karen Woog, Martin A. Makaryb, and Caitlin W. Hicks
Reference: European Journal of Vascular and Endovascular Surgery - Available online 19 June 2024
DOI: 10.1016/j.ejvs.2024.06.017
Read the abstractObjectives:
To evaluate whether infrapopliteal PVI is associated with worse long-term outcomes compared with isolated femoropopliteal PVI for the treatment of claudication.
Population:
Retrospective cohort study, multicenter, including 36,147 patients with claudication. Exposure was any index infrapopliteal PVI, including both infrapopliteal PVI in isolation and infrapopliteal PVI with concomitant femoropopliteal PVI, compared with index isolated femoropopliteal PVI
Endpoints:
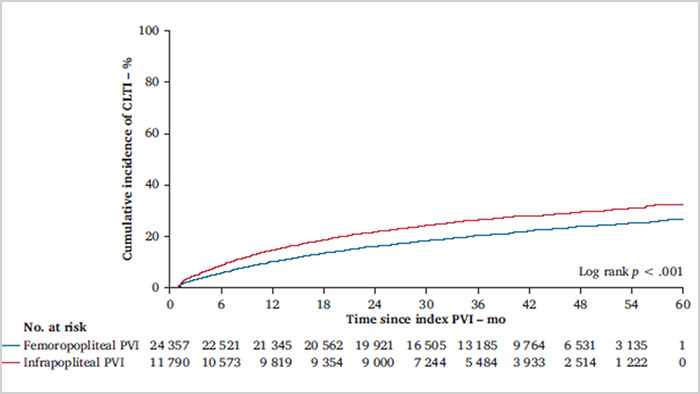
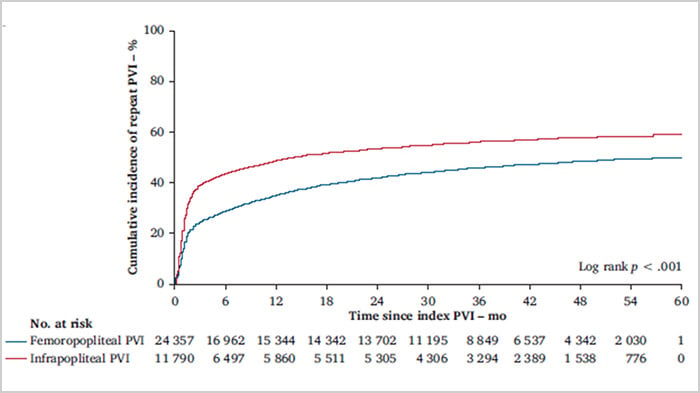
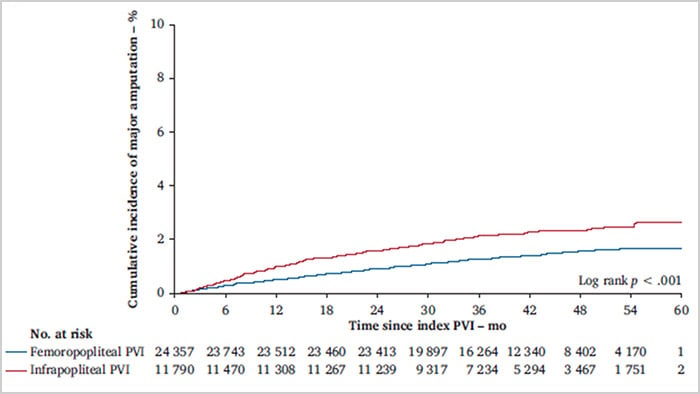
Conversion to CLTI, any repeat PVI, and major amputation.
Outcomes and conclusion:
Among Medicare beneficiaries in the USA who underwent an infra-inguinal PVI to treat claudication, infrapopliteal PVI was associated with worse long term outcomes compared with isolated femoropopliteal PVI.
Get the latest clinical cases and breaking news delivered straight to your inbox!


Comments: