An outpatient pharmacist strategy improves guideline adherent medication prescribing in patients with vascular disease
Selected in ESVS Journal by Guillaume Nicaud
Vascular diseases such as LEAD, carotid stenosis, AAA, and TAA carry high morbidity and mortality. Best medical treatment (BMT)—including statins, antiplatelet therapy, and smoking cessation—is essential, yet guideline adherence remains low: statins 30–80 %, antiplatelets 30–95 %, smoking cessation counseling 15 %, and pharmacological treatment 10 %.
Pharmacist-led interventions may improve prescription and adherence to BMT, reduce costs, and free specialist time. Evidence from cardiology and vascular medicine supports their effectiveness, but real-world data in patients with vascular diseases are limited.
This study evaluated the impact of pharmacist review on BMT prescription, focusing on statins, antiplatelet therapy, and smoking cessation interventions.
References:
Authors: Aaron Tran, Alexandra Lotric, Lauren Hunt, Thodur Vasudevan
Reference: Published online March 21, 2025 - Presented at the Thirty-ninth Annual Meeting of the Western Vascular Society, Colorado Springs, CO, September 7-10, 2024.
DOI: DOI: 10.1016/j.ejvs.2025.07.014
Read the abstractBackground:
Statins, antiplatelet therapy, and smoking cessation are proven to reduce morbidity and mortality in patients with peripheral arterial disease (PAD), carotid stenosis, and abdominal aortic aneurysm (AAA).
According to the 2024 ESVS guidelines, antiplatelet therapy is recommended for symptomatic PAD, for carotid stenosis greater than 50 %, and for AAA, while statins are advised for all patients with PAD (even asymptomatic), carotid stenosis, and AAA. Smoking cessation is strongly recommended for all.
Objective:
The objective of this study was to evaluate the impact of a specialised outpatient pharmacist on the initiation of best medical treatment (BMT)—including statins, antiplatelet therapy, and smoking cessation—in patients with vascular disease.
Methods:
Population:
- Patients with PAD, carotid stenosis, abdominal aortic aneurysm (AAA), or thoracic aortic aneurysm (TAA) were eligible for statin and antiplatelet therapy review.
- All patients consulting in the vascular clinic were assessed for smoking status and cessation needs.
Eligibility for pharmacist review (≥ 1 required):
- First consultation in the vascular clinic
- Missing or insufficient best medical therapy (statins, antiplatelet therapy, smoking cessation)
- Need for anticoagulation/antiplatelet regimen review
- History of medication non-adherence
- Medication-related adverse effects
- Multiple vascular risk factors (hypertension, diabetes, coronary artery disease, stroke)
- Current smoking status
- Recent smoking cessation
Study endpoints:
- Primary: initiation of statins and antiplatelet therapy in accordance with guidelines
- Secondary: smoking cessation interventions, including nicotine replacement prescription
Outcomes:
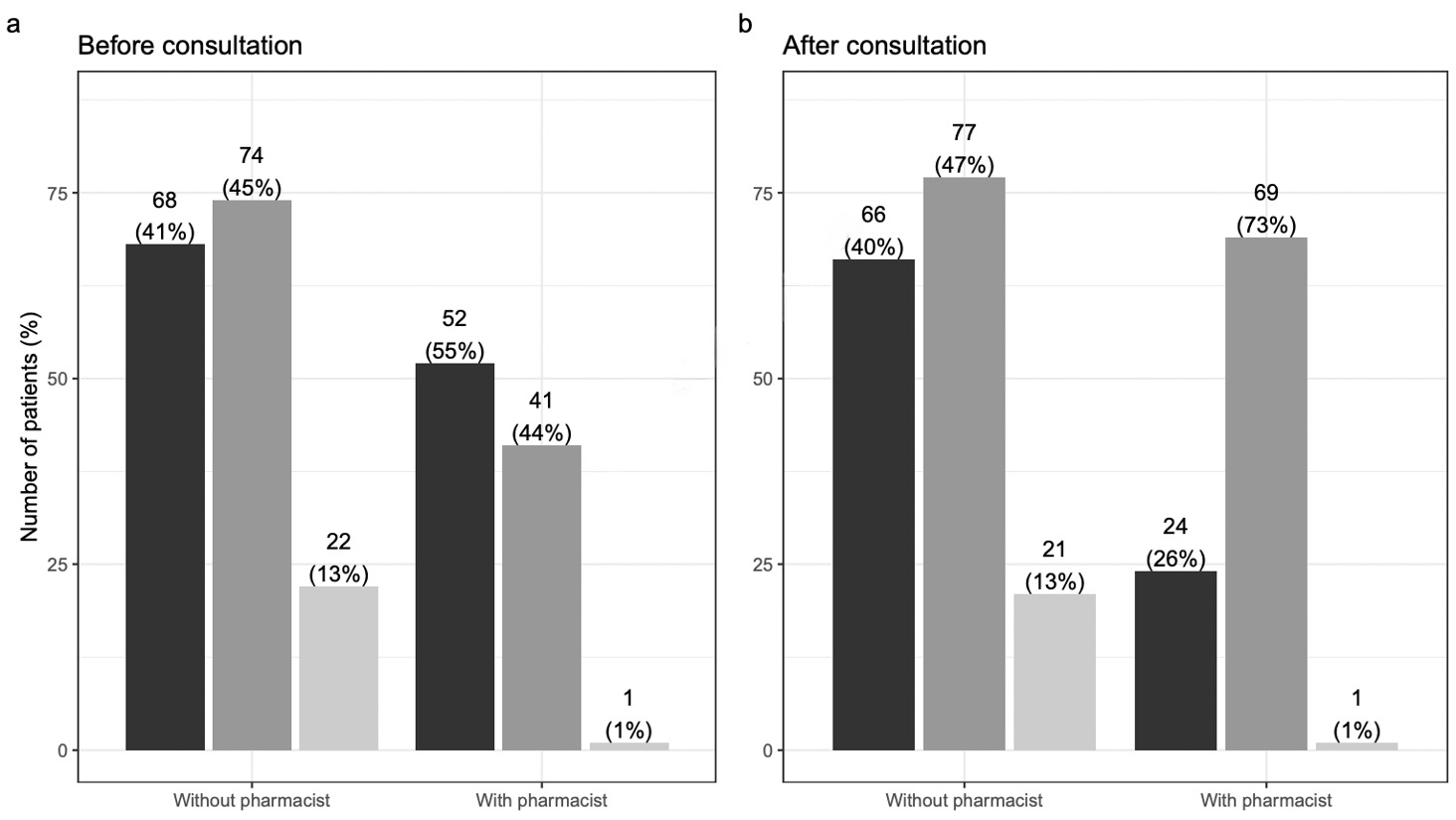
- Population: 258 patients included in statin and antiplatelet analyses (pharmacist review: 94; no pharmacist review: 164).
- Statins: pharmacist review was associated with higher-intensity statin prescribing (AOR 3.38, 95 % CI 1.71–6.67; χ²LR = 13.58, df = 1, p < .001).
- Antiplatelet therapy: no statistically significant association with pharmacist review (AOR 0.66, 95 % CI 0.30–1.46; χ²LR = 1.06, df = 1, p = .30).
- Smoking cessation (107 smokers):
- Nicotine replacement therapy prescription increased with pharmacist review (unadjusted OR 3.98, 95 % CI 1.38–11.52; χ²LR = 7.05, df = 1, p = .008).
- Referral to smoking cessation services markedly increased (unadjusted OR 19.20, 95 % CI 4.14–89.01; χ²LR = 23.65, df = 1, p < .001).
Get the latest clinical cases and breaking news delivered straight to your inbox!


Discussion:
This study suggests pharmacist improve initiation of statins and smoking cessation, but not antiplatelet therapy, likely due to high baseline APT use, limited sample size, and cautious pharmacist practices.
The BMT intervention appears relevant given low adherence to guideline-recommended therapies in PAD: statins 30–80 %, APT 30–95 %, smoking cessation counseling 15 %, and nicotine replacement 10 %.
Similar studies show pharmacist-led interventions improve BMT initiation and adherence in cardiology. An other one show comparable results for statins in peripheral arterial disease and aneurysm subgroups.
Limitations include retrospective control data, limited covariates in multivariate analyses, monocentric design, lack of data on actual smoking cessation, BMT adherence, and potential selection bias toward more severe patients.
Conclusion:
Best medical treatment (BMT)—including statins, antiplatelet therapy, and smoking cessation—is essential in the management of vascular diseases such as LEAD, carotid stenosis, AAA, and TAA.
Despite clear guideline recommendations, BMT remains underprescribed, particularly in patients with peripheral arterial disease: statins 30–80 %, antiplatelets 30–95 %, smoking cessation counseling 15 %, and pharmacological smoking cessation treatment 10 %.
Pharmacist-led interventions appear to improve prescription to BMT, and probably its adherence, reduce healthcare costs, and free up valuable time during specialist consultations.