PVI Trials book 2023
Are you ready to elevate your practice with the groundbreaking PVI Trials book? Dive into the latest trials, gain valuable insights, and stay at the forefront of vascular surgical and endovascular techniques!
Unleash the Power of Data: Introducing the PVI Trials Book 2023!
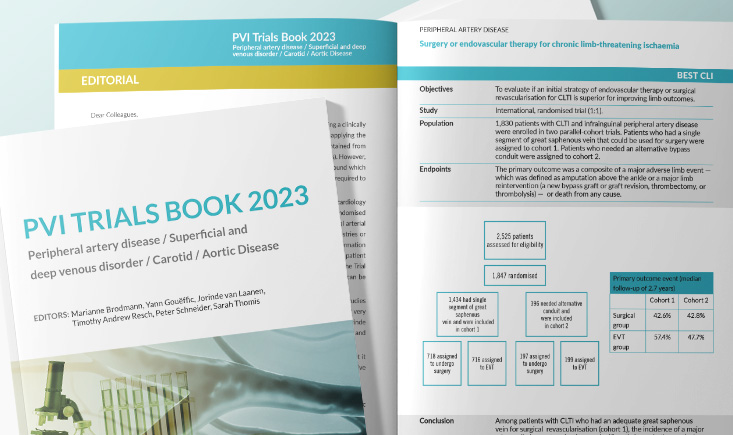 The creation of this Trials Book is inspired by what is already being done in interventional cardiology and interventional neurology. It will consist in a corpus of one-page summaries of published randomized trials and meta-analysis in 5 domains of expertise: aorta, carotid, peripheral arterial disease, vein and embolization.
The creation of this Trials Book is inspired by what is already being done in interventional cardiology and interventional neurology. It will consist in a corpus of one-page summaries of published randomized trials and meta-analysis in 5 domains of expertise: aorta, carotid, peripheral arterial disease, vein and embolization.
Marianne Broadmann (peripheral arterial disease), Sarah Thomis (vein), Jorinde Van Laanen (embolization), Tim Resch (aorta) and Peter Schneider (carotid) editors of this new edition, have gathered the most significant trials in this must-have guide.
Get the full trial books for free!
Discover exclusive preview trials!
To give you an overview of the trials book, we are pleased to offer you access to a selection of them.
You must be logged in or create an account to see all the content
I have my account
Not registered yet? Create your account and get free access to:
- Access slide presentations from PVI
- Watch session videos and cases
- Discuss cases with your peers
- Register for and view PVI
- Read a selection of articles
- And more…
