Patient-tailored endovascular therapy of the thoracic aorta
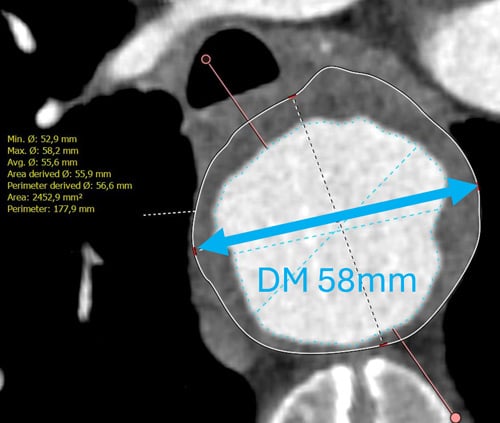
This challenging case features a 65-year-old patient with multiple comorbidities, a 58 mm thoracic aneurysm, and a severely kinked, diseased aorta.
Key questions include configuring the optimal proximal landing zone, navigating complex anatomy during endovascular repair, and reducing the risk of spinal cord ischemia.
Patient / Anatomy
- A 65-year-old male patient.
- Extensive coronary artery disease – PCI to RIM; chronic total occlusion of RCA.
- Smoking history: 50 pack-years.
- COPD.
- Type 2 diabetes mellitus.
- CKD II.
- Severe depression.
- Hyperlipidemia (HLP).
- Progressive aneurysm, diameter 58 mm.
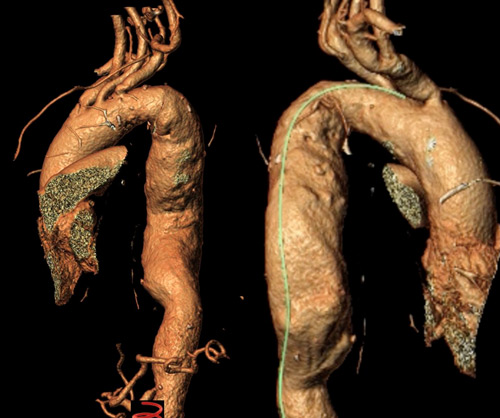
- Kinked anatomy (proximal descending!).
- Diseased aorta and Iliac arteries.
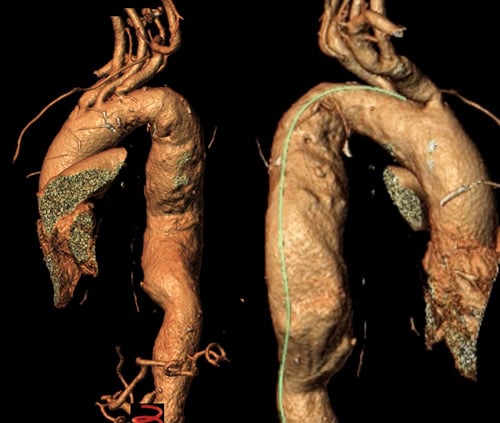
Distal Arch / Proximal descending
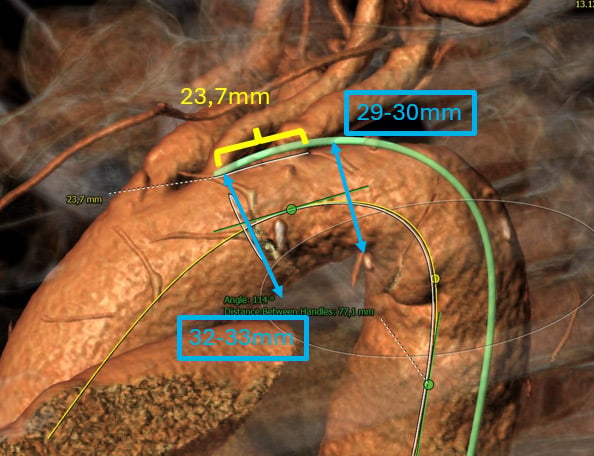
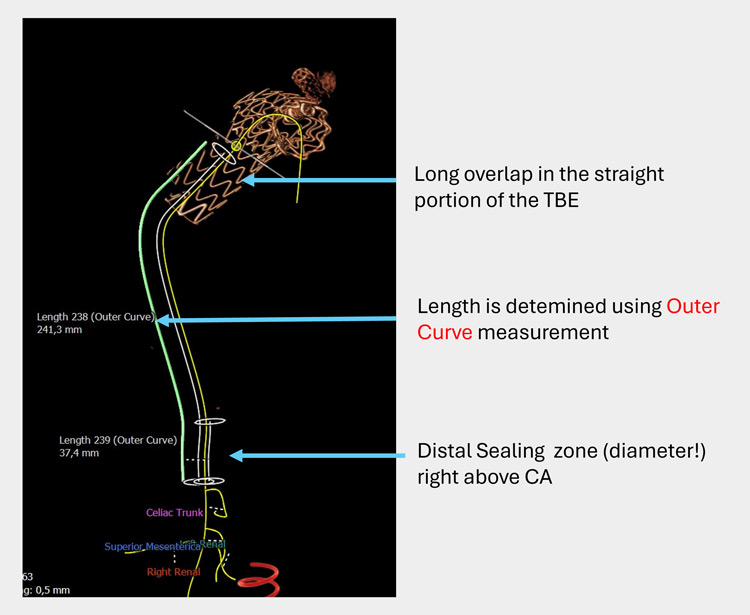
Length & extent
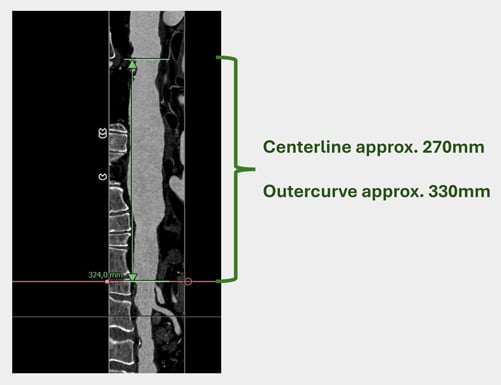

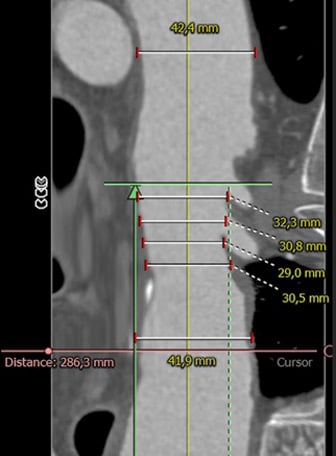
Distal landing zone
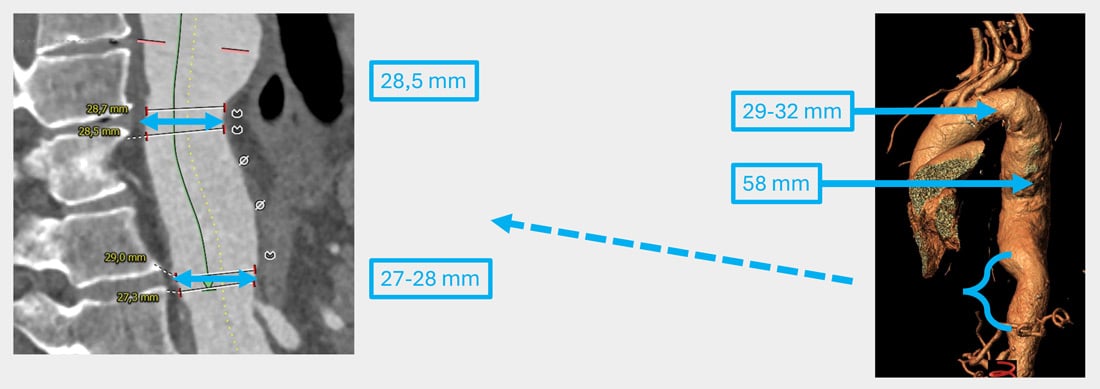
Proximal sealing concept
- From our perspective, adequate proximal sealing is feasible with a branched solution.
- We always try to preserve the left subclavian artery.
- In this case, we propose the GORE® TAG® Thoracic Branch Endoprosthesis (TBE) as an off-the-shelf option with good conformability to kinked aortic pathology.
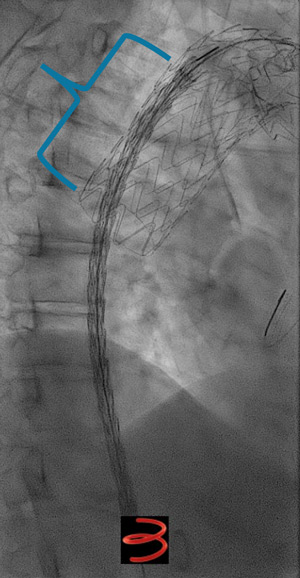
Step 1
GORE® TAG® Thoracic Branch Endoprosthesis (TBE)
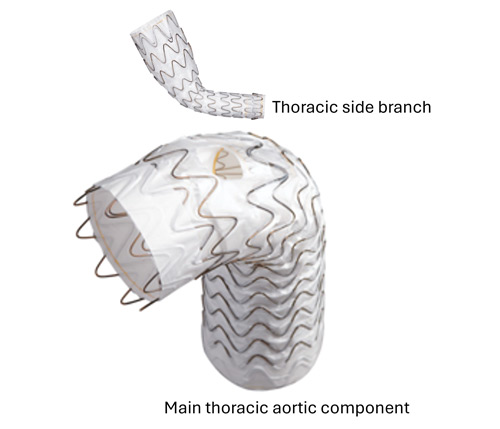
Challenging branch take-offs may require specific angulations!
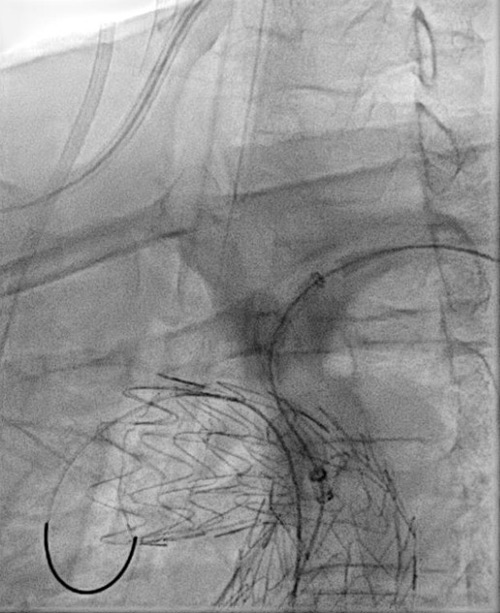


Step 1: result

Staged approach for spinal cord protection
- Planning of a staged procedure to minimise the risk of spinal cord ischaemia.
- TBE in 1st step followed by two TEVAR components after 8 weeks.

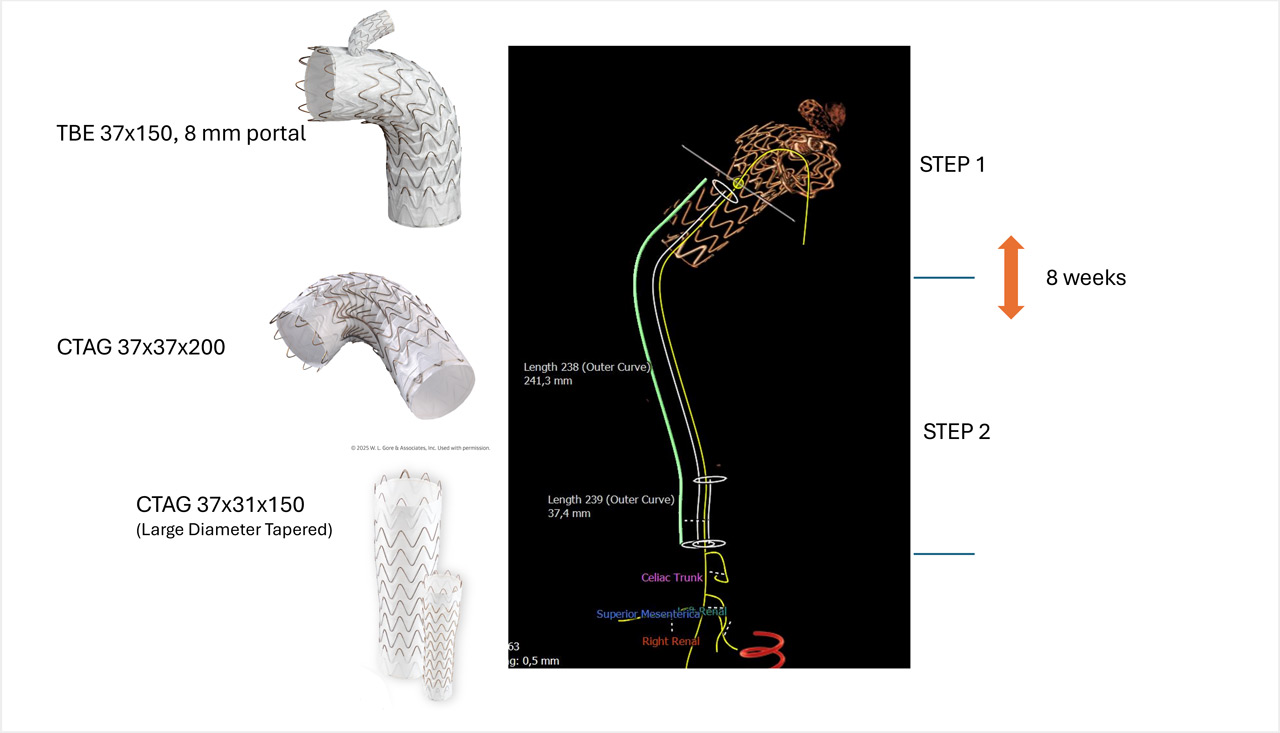
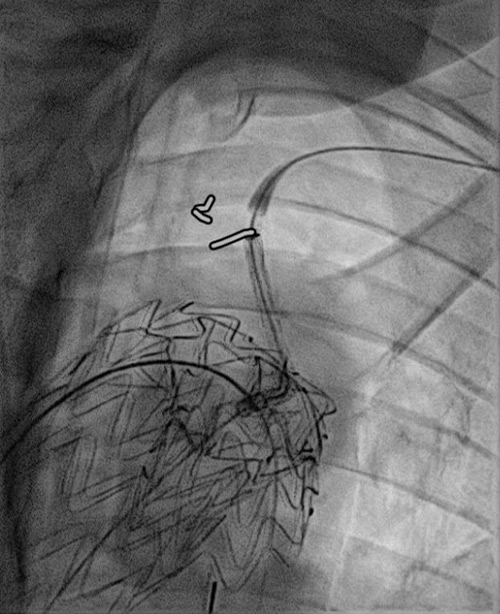
Step 2 (after 8 weeks):
Distal optimisation and future treatment option
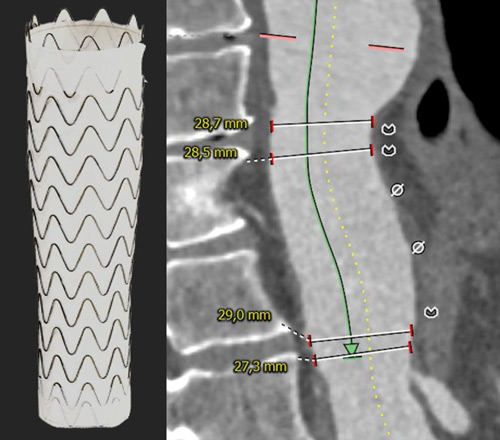
- Further extension of the 37 x 200 mm Gore® TAG® Conformable with a large diameter tapered 37/31 x 150 mm TAG® Conformable
- At the same time, preparation for a potential later extension into the abdominal aorta, should the disease progress and become treatment-indicated in this segment.
- Reduction of the risk of a distal stent graft–induced new entry (dSINE) and improved adaptation to the patient’s anatomy.
37 TAG® Conformable in 37 TBE -> Long overlap!
Staged deployment of the tapered TAG® Conformable with precise control of the distal landing zone.
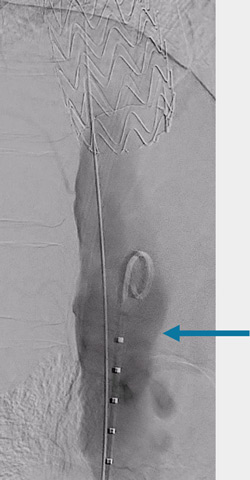
Ballooning under controlled hypotension with a Tri-Lobe balloon.

- No peri-operative complications.
- Uneventful hospital course.
- No neurological events.
- Uneventful follow-up.

Conclusions
- Branched and tapered endovascular solutions can optimise both proximal and distal sealing zones.
- Tapered stent-graft configurations may reduce wall-stress–related stent graft–induced new entry (SINE).
- Both concepts enable an endovascular repair strategy tailored to the individual patient’s anatomy and pathology.
- Tapered solutions provide an additional option to facilitate future extensions without the need for further custom-made components.
Concept / Strategy Overview
Proximal sealing concept
- Multimorbid patient – endovascular approach is proposed.
- Proximal sealing zone is limited.
- Adequate proximal sealing is considered achievable with a branched solution.
- Proposed device: GORE® TAG® Thoracic Branch Endoprosthesis (TBE).
- Advantages: off-the-shelf availability and good conformability to kinked aortic pathology.
Two-stage approach for spinal cord protection
- Planning of a staged procedure to minimise the risk of spinal cord ischaemia.
Patient-specific anatomical adaptation / distal optimisation and future treatment option
- Adaptation to the patient’s individual anatomy by extending the 37 mm TBE with an additional 37 mm TAG® Conformable with long overlap.
- Further extension of the 37 mm TAG® Conformable with Large Diameter Tapered TAG® Conformable to match the distal aortic diameter.
- At the same time, preparation for a potential later extension into the abdominal aorta, should the disease progress and become treatment-indicated in this segment.
- Reduction of the risk of a distal stent graft–induced new entry (dSINE) and improved adaptation to the patient’s anatomy.
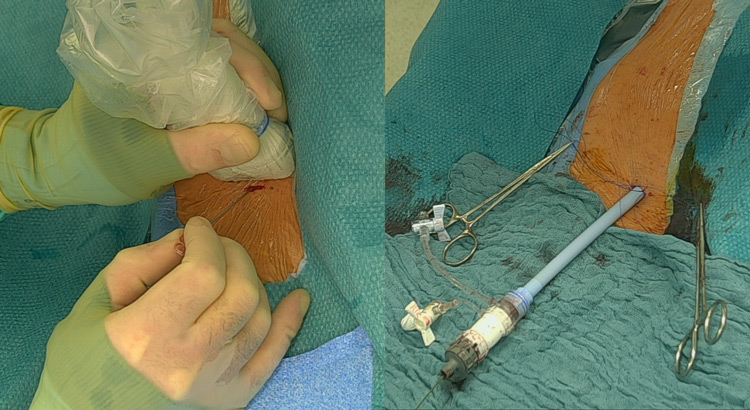
Access strategy and procedural technique
- Both procedures are performed completely percutaneously with ultrasound-guided access and use of a preclose technique.
- This optimises the staged approach and reduces the risk of access-vessel complications.
Dr. Florian Elger: workshops and speaker for W.L. Gore, workshops and proctor for Terumo Aortic
Supported through an unrestricted educational grant from Gore
![]()
Get the latest clinical cases and breaking news delivered straight to your inbox!

