Impact of socioeconomic wealth on chronic limb-threatening ischemia revascularisation outcomes among Medicare patients from 2016 to 2023
Selected in Journal of Vascular Surgery by Léna Lemouzy
This multicentric retrospective study evaluated over 330,000 Medicare beneficiaries undergoing endovascular revascularisation for CLTI between 2016 and 2023.
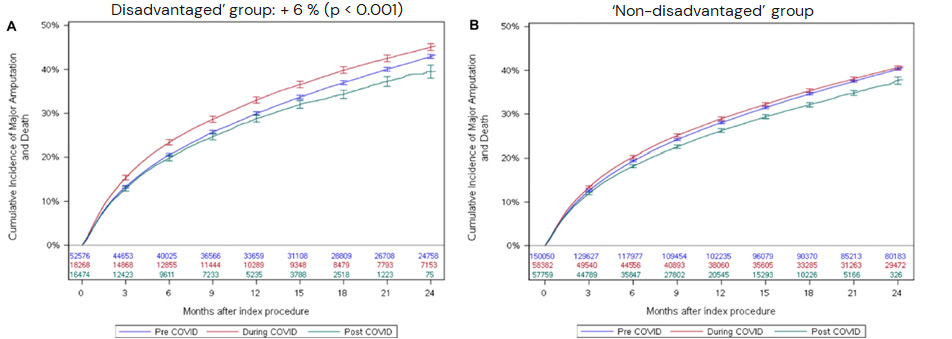
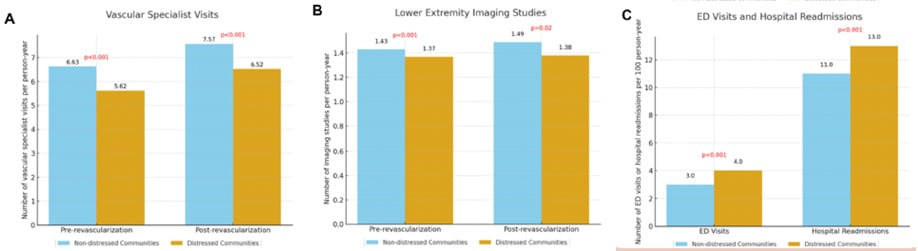
Patients from socioeconomically distressed regions faced higher risks of major amputation and post-procedural mortality, fewer consultations with vascular specialists, and increased emergency visits and hospital readmissions—trends amplified during the COVID-19 pandemic.
The findings highlight persistent disparities in CLTI care and suggest the need for targeted interventions to improve access and outcomes in vulnerable populations.
References:
Authors: Maxime Dubosq-Lebaz, Joseph M Kim, Siling Li, Frank Medina, Manon Jouffroy, Marc L Schermerhorn, Yann Gouëffic, Eric A Secemsky
Reference: Published online August 28, 2025
DOI: 10.1016/j.jvs.2025.08.029
Read the abstractBackground:
Chronic limb-threatening ischemia (CLTI) carries high risks of major amputation and mortality despite revascularisation.
Socioeconomic disparities may influence access to care and clinical outcomes, but data evaluating these effects across U.S. regions, particularly before, during, and after the COVID-19 pandemic, remain limited.
Objective:
To assess the association between regional socioeconomic status, measured by the Distressed Communities Index (DCI), and CLTI-related outcomes—including mortality, major amputation, and repeat interventions—in Medicare beneficiaries undergoing peripheral revascularisation.
Method:
This multicenter, retrospective observational study included 333,173 Medicare beneficiaries who underwent endovascular revascularisation for CLTI between January 1, 2016, and December 31, 2023.
Patients were categorised into “distressed” (DCI ≥ 80 %; 66,757 patients) and “non-distressed” (266,416 patients) groups. Data were extracted from Medicare claims and national databases, including socioeconomic indicators. Mean follow-up was 663 days.
Primary outcome was a composite of major amputation and all-cause post-revascularisation mortality. Secondary outcomes included reintervention and healthcare utilisation indicators.
Outcomes:
Patients from distressed areas had a significantly higher risk of major amputation and all-cause mortality (+ 3 %) compared with non-distressed patients throughout the study period. The disparity widened during the COVID-19 pandemic and remained substantial afterward.
These patients also had fewer consultations with vascular surgeons and fewer vascular imaging studies, but more emergency department visits and hospital readmissions related to CLTI.
No significant differences were observed regarding reintervention rates.
Get the latest clinical cases and breaking news delivered straight to your inbox!


Discussion:
This study has several limitations:
The association between low socioeconomic status (SES) and worse cardiovascular outcomes is multifactorial:
These findings highlight the importance of targeted strategies to reduce disparities:
Conclusion:
Socioeconomic distress is associated with worse outcomes after CLTI revascularisation, reflecting disparities in access to specialist care and imaging.
The COVID-19 pandemic further amplified these inequities, highlighting a persistent public health concern and the need for targeted strategies to improve care in vulnerable populations.