Safety and efficacy of rotational thrombectomy and drug-coated balloon angioplasty in patients with femoropopliteal in-stent restenosis and occlusions
Selected in ESVS Journal by Mohammed Alotaibi
Femoropopliteal in-stent restenosis (ISR) remains a challenging complication after endovascular treatment, particularly in long and occlusive lesions.
While drug-coated balloon (DCB) angioplasty is an established therapy, its effectiveness may be limited in complex ISR due to high thrombotic burden and restricted luminal gain.
Rotational thrombectomy with the Rotarex S system offers effective lesion debulking and may optimise vessel preparation before DCB angioplasty.
This study evaluates the safety and 12-month efficacy of Rotarex S thrombectomy followed by DCB angioplasty in patients with complex femoropopliteal ISR.
References:
Authors: Martin Andrassy, Safeer A. Najam, Dalibor Dukic, Amila Jehn, Christoph Schöfthaler, Grigorios Korosoglou
Reference: Published online June 18, 2025
DOI: DOI: 10.1016/j.ejvs.2025.06.021
Read the abstractObjective:
The aim of this study was to evaluate the safety and efficacy of rotational thrombectomy using Rotarex S followed by drug-coated balloon (DCB) angioplasty for the treatment of femoropopliteal in-stent restenosis (RIS).
Study:
Prospective, observational bicentric study conducted in two vascular centres between January 2017 and August 2023, including patients treated with Rotarex S debulking followed by DCB angioplasty for femoropopliteal in-stent restenosis.
Population:
215 patients with symptomatic femoropopliteal in-stent restenosis
- Rutherford class 2-5
- Osaka II (23.3 %) and Tosaka III (76.7 %) lesions
- Median lesion length: 22.0 cm
Endpoints:
- Primary endpoint: primary patency at 12 months
- Secondary endpoint: freedom from clinically-driven target lesion revascularisation (CD-TR)
- Safety endpoint: procedural complications
Outcomes:
This prospective two-centre study demonstrates strong procedural efficacy and a favourable safety profile for rotational thrombectomy followed by drug-coated balloon (DCB) angioplasty in patients with femoropopliteal in-stent restenosis and occlusions.
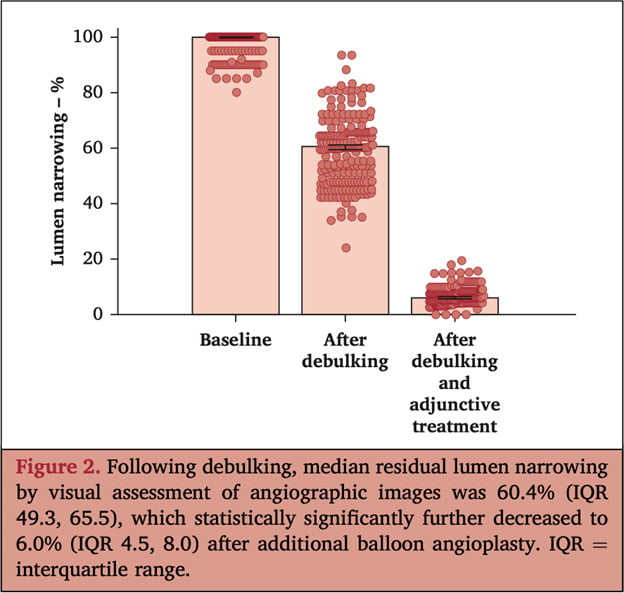
At baseline, lesions were nearly completely occluded. Rotational thrombectomy significantly reduced stenosis to a median residual of 60.4 %, which was further optimised to 6.0 % after DCB angioplasty, corresponding to a 94 % luminal gain from total occlusion to vessel patency. Procedural success was achieved in 100 % of cases.
The safety profile was excellent, with no vascular perforations and a low rate of peripheral embolisation (1.4 %), all of which occurred in subacute total occlusions and were successfully managed intra-procedurally using aspiration catheters. No distal protection devices were used. There were no major amputations, no procedure-related deaths, and no need for surgical conversion. Access-site complications were infrequent and manageable.
At 12 months, primary patency was 79.2 %, with freedom from clinically driven target lesion.
Get the latest clinical cases and breaking news delivered straight to your inbox!


Discussion:
This two-centre, prospective study highlights the efficacy of combining Rotarex thrombectomy with drug-coated balloon (DCB) angioplasty for complex femoropopliteal in-stent restenosis. The standardised protocol and thorough 12-month imaging follow-up are notable strengths, demonstrating that this approach is viable in experienced centres, especially for Tosaka II–III lesions.
However, the study has limitations, including the absence of a comparator group and potential selection bias. The diversity of DCB devices and the 12-month follow-up period may overlook late events. While informative, further randomised controlled trials are needed to confirm its superiority over other methods.
Alternative strategies include DCB alone, laser atherectomy with DCB, covered stents, and bypass surgery. Future research should focus on long-term outcomes and cost-effectiveness.
Conclusion:
Rotational thrombectomy using Rotarex S followed by DCB angioplasty is a safe and effective treatment for complex femoropopliteal in-stent restenosis, including long and occlusive lesions.
At 12 months, the strategy achieved 79.2 % primary patency and 95.1 % freedom from CD-TLR, with an excellent safety profile and low complication rates.