Cases and resources in vascular techniques
This section provides a selection of cases and resources provided by experts in vascular techniques.
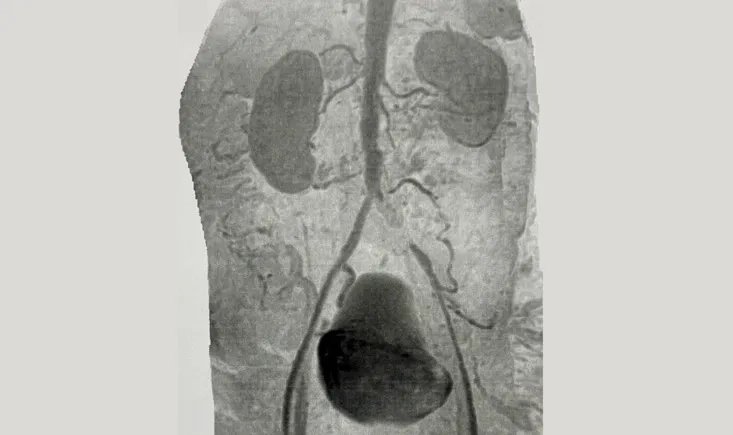
This case explores the management of a unilateral total iliac artery occlusion in a high-risk patient with advanced peripheral arterial disease. Through imaging findings and clinical presentation, it invites reflection on treatment options, weighing endovascular and surgical strategies in the context of symptom severity, collateral circulation, and overall cardiovascular risk.
At PVI 2025, Claire Webster explores the impact of social media on vascular surgery: its educational value, its risks, and the responsibility that comes with sharing cases online. A concise look at how digital platforms can support practice without replacing human interaction.
At PVI 2025, Dr. Piotr Musialek explains how carotid stenting has evolved from simple stent placement to a precise approach: rigorous lesion preparation, pre- and post-dilatation, and full vessel optimisation. The PARADIGM-500 study shows this strategy reduces in-stent restenosis and eliminates stent thrombosis compared with earlier-generation techniques.
This PVI webinar replay explores complex EVAR cases. Prof. Verhoeven presents 10-year GREAT Registry outcomes, Prof. Bicknell shares CLEVAR Registry insights on hostile necks, and Prof. Yeung highlights long-term registry data. Lively discussions and live audience questions reveal practical guidance for everyday decision-making.
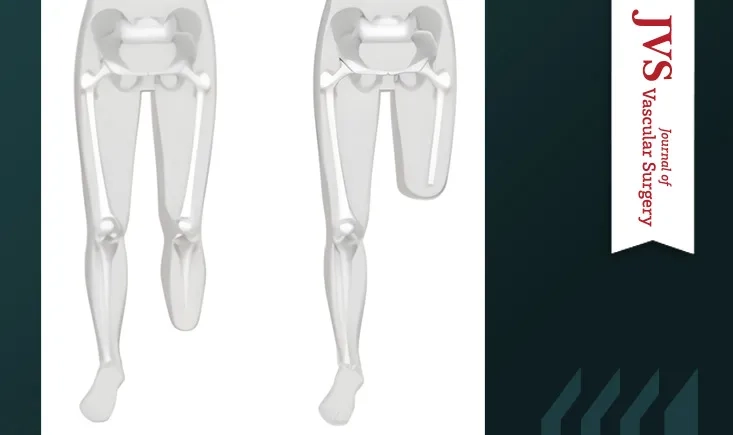
Nearly one in four below-knee amputations required revision. In this cohort of 212 patients, profunda femoris patency was the strongest predictor of stump healing, whereas prior revascularisation did not reduce revision risk, underscoring the importance of preoperative inflow assessment.
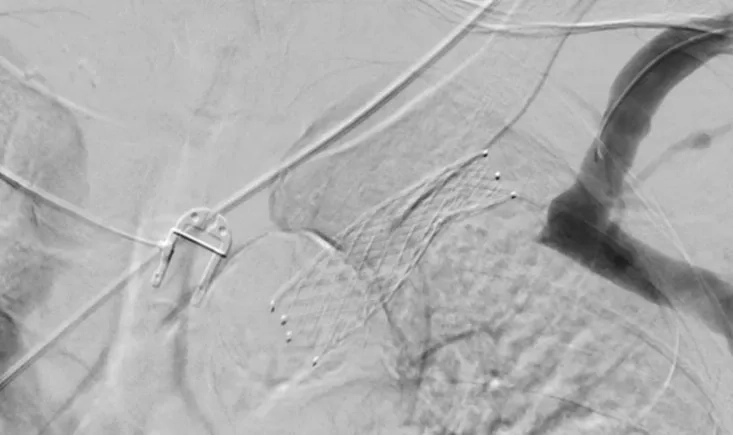
This case explores the management of a complex subclavian vein intra-stent occlusion in a haemodialysis patient, raising key questions when standard endovascular options reach their limits.
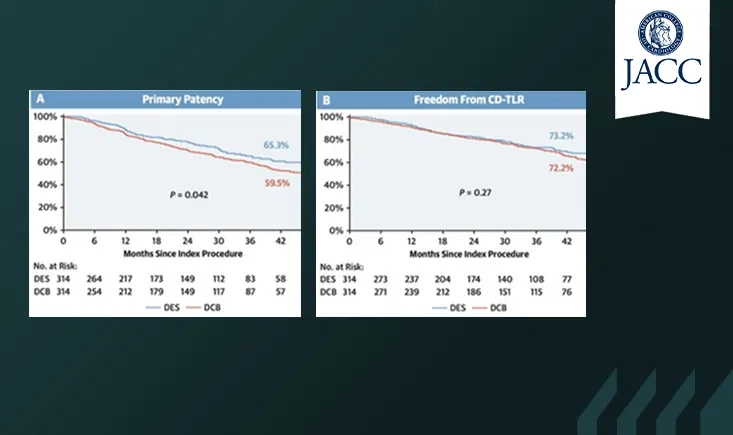
The BEASTARS data suggest that, even after optimal lesion preparation, the superior patency of DES over DCB does not translate into better clinical outcomes, challenging how success is defined in femoropopliteal interventions.
Prof. Peter Schneider discusses the role of transcarotid artery revascularisation (TCAR) in high-risk carotid disease, focusing on patients with recent symptoms and contralateral carotid artery occlusion. Drawing on large real-world data, he reviews outcomes compared with carotid endarterectomy and transfemoral stenting, and highlights where TCAR fits in contemporary practice.
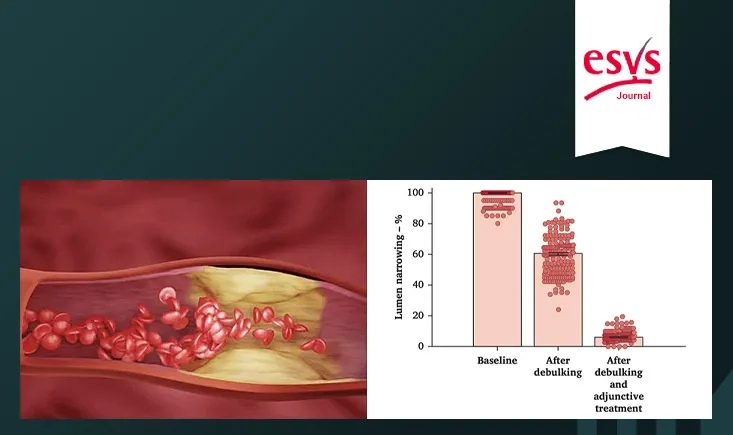
The aim of this study was to evaluate the safety and efficacy of rotational thrombectomy using Rotarex S followed by drug-coated balloon (DCB) angioplasty for the treatment of femoropopliteal in-stent restenosis (RIS).
Prof. Secemsky explains how medico-administrative databases are transforming research and decision-making in lower-extremity arterial disease. Real-world evidence complements limited clinical trial data, helping clinicians navigate safety challenges and better understand device performance in complex patient populations. This interview explores how multiple data sources can guide practical, patient-centered decisions for emerging therapies.